Let’s start with a few givens (i.e. things that are well documented and known):
- Cortisol is the “stress” hormone. It is good in small amounts (getting you up in the morning, running away from lions) and bad in the chronic long term (immune suppression, abdominal “beer belly” obesity).
- Serotonin is the regulator of the six F’s: Fight, Flight, Food, Falling asleep, Feeling good, and… Sex. Too much is bad too little is bad. The same story as cortisol.
- Serotonin is involved in regulating cortisol secretion by the 5-HT(2a/2c) receptors (more serotonin, less cortisol)
Let’s step into the much neglected world of serotonin research on obesity. When’s the last time you’ve heard in pop culture about serotonin in any other way than depression? Maybe I’m reading the wrong news sites but the interplay here is important, however rarely talked about.
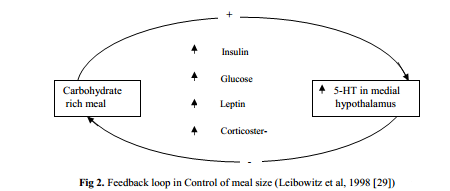
Serotonin has a strong entanglement with carbohydrate consumption. Additionally, carbohydrates significantly raise blood plasma levels of tryptophan. This tryptophan is then transported into the brain and is the precursor for serotonin. In a normally functioning system this would cause satiety, as it increases serotonin levels (and lowers cortisol).
It also turns out there are different polymorphisms for the serotonin receptor modulating cortisol. The lucky homozygotes for the -1438G allele had increased body mass and abdominal distribution of body fat along with less suppression of cortisol with dexamethasone than the other genotypes.
It seems serotonin could be a huge mechanism for failure. A disorder in producing serotonin could lead to the overconsumption of carbohydrates with little to no satisfaction (but the craving sensation would linger). An issue with the serotonin receptor modulating cortisol (or too little serotonin in the first place) could mean that despite a rich carbohydrate meal, the cortisol levels would never respond- leading to the unfortunate and unnecessary sequestering of fat. Dieting and food scarcity, while at first may seem like a good idea for dieting, does significantly boost cortisol levels and lead the vicious regain of weight once one strays from the path. Indeed, when given antidepressants that work on promoting serotonin bioavailability, it reduces food intake and circulating cortisol levels. One paper even concludes:
[…] there is evidence that some selective serotonin reuptake inhibitors are effective as antiobesity drugs.”
But before you rush out to get some Prozac, it’s important to realize that all of this is a function of eating carbohydrates. I have been searching, but it has been difficult to find and prove my theory here- that going low carb rehabilitates the serotonin system. This paper seems to have an extremely positive association between low carb diets and better sleep, mood, and memory (functions relating to serotonin). Also because most low carb advocates will stand by the idea of eating until you’re full- there is no starving cortisol mechanism kicking in- thus helping the body recover from cortisol overproduction.
It’s at least food for thought… 😉
Resources
- 5-HT2A Receptor Gene Promoter Polymorphism in Relation to Abdominal Obesity and Cortisol, Rosmond, Bouchard et al. Obesity Research, Volume 10, Issue 7, pages 585–589, July 2002.
- Effects of normal meals rich in carbohydrates or proteins on plasma tryptophan and tyrosine ratios, Wurtman, Wurtman et al. American Journal of Clinical Nutrition, January 2003 vol. 77 no. 1 128-132.
- Long-term Effects of a Very Low-Carbohydrate Diet and a Low-Fat Diet on Mood and Cognitive Function, Brinkworth, Buckley et al. JAMA Internal Medicine. 2009;169(20):1873-1880. doi:10.1001/archinternmed.2009.329.
- Regulation of Appetite: Role of Serotonin and Hypothalamus, Sharma and Sharma. Iranian Journal of Pharmacology. Vol 11, 2, 2012.

Certainly food for thought. I wonder if a disbalanced serotonin system isn’t partly responsible for the depression I felt for so many years.
Ooooh… I found myself wondering if it works the other way: chronic overconsumption of carbohydrates leads to serotonin disregulation… and the consequences thereof ensue…
Inflammation seems to be a big part of depression as well, so look at whats causing inflammation in your body to help depression.
I had a long history of depression/dysthymia/binge eating. Eating Low Carb seems to enable me to manage my binge eating & compulsive eating really well. A couple of weeks ago I remembered about 15 years ago going on a VLC and low calorie, low fat diet and within about 7 days becomes profoundly depressed until a friend finally said “for god sake eat a potato!” I was wondering why haven’t experienced that this time (I think because I’m eating high fat/mod protein) I’ve been lLC for almost 2 years now…no major symptoms of depression, no carb cravings. Adaptation?
Question: I started good solid Ketosis at the first of January and my blood pressure (which went down when I first started LC and stayed down until the past few months) shot back up to the 140/90 range…cortisol? I’m hoping if it is related to the Ketosis, it will resolve soon. I can find almost no examples of other people having this experience- most say that Ketosis improved their BP.
Hi Kim!
Maybe Karin will have some insight into this, but unfortunately I’ve not heard of blood pressure correcting and then rebounding like that as a consequence of a ketogenic diet.
Your cortisol question is intriguing, but it’s not something I know enough about to comment on (or at least, have a comment worth reading).
I’d love to learn more about this. If you get an explanation, will you share it with us?
-Michael
Some things to consider would be histamine, because it’s a vasodilator…and also the minerals like magnesium and potassium because they’re harder to get on a keto diet. Also worth thinking about multiple measurements with bp: you should be sitting down for at least 15 minutes before measuring and should repeat each time under the same conditions to get an accurate reading. Adrenaline is also a strong vasodilator in periferal parts of the body, so cold feet, hands can also be a clue. The keto diet may be stressful to the body during thr adaption phase.
It’s interesting to see that SSRI’s are as effective as anti-obesity drugs. My experience was just the oposite. When I was on Paxil, I wanted to do nothing but eat and sleep. I also got cravings for alcohol. Getting off them was a nightmare as well.
I’ll stay ketogenic, thank you. 🙂
Your understanding of serotonin is inadequate.
I would like to see some research on ketogenic diet and sexual orientation. Some recent research shows that low serotonin is implicated in homosexuality and chronic high carb diets usually cause low serotonin. The ketogenic diet would reverse the serotonin receptors burn-out. I think the keto diet should be seasonal, only during winter. Upon re-introduction of carbs (but not high glycemic index ones like sugar, honey) the LGBT would get a boost of sexuality and would change sexual orientation.
Regardless of whether it’s beneficial for some. I would suspect this not to be the case for everyone. Going keto resulted in depression and fatigue-like symptoms for me personally. My guess is the epigenetic links haven’t been well studied in nutritional research in terms of Keto. There is no one size fits all or silver bullet.